By Joyce Kyles, strategic solution speaker, storyteller, writer, life and thriving skills coach, and consultant
Domestic and sexual violence and other lifetime trauma can have significant mental health consequences. Yet, many systems and services available are often unprepared to help survivors address and heal from the traumatic effects of abuse. In addition, survivors within marginalized communities are not as likely to discuss, report, or seek help for their mental health and mental illness.
For the past 20 years, I have learned a lot from the communities that I have worked with. Whether working with individuals, nonprofits, the military, law enforcement, women, teens, faith-based communities, businesses or organizations, my goal has always been to provide realistic and practical solutions while having my audiences and clients consider thought provoking accountability and action.
In this Technical Assistance Question of the Month, I share recommendations and tangible resources to help advocates in the gender-based violence movement better support survivors within marginalized communities in addressing their mental health needs. These include: 1) understanding mental health versus mental illness; 2) addressing the psychological effects of domestic and sexual violence; 3) advocating for more funding; 4) providing survivors and advocates with safe spaces for mental health support, and 5) increasing the focus on awareness and treatment of marginalized survivors.
“To me, mental health means the quality of life and the ability/opportunity to have a balanced and fulfilled sense of self.” – Savanna Karmue (she/her), Sacramento, CA, age 16
Systemic issues and barriers within the health care system, such as access and cost, have disproportionately affected marginalized groups. For example, Black Americans identify the following as ten of the biggest barriers to seeking and accessing mental health help:
- High costs of mental health care
- Familial shame around mental health
- Cultural stigma of mental illness
- Lack of diversity in health care
- Poor competency among non-Black clinicians
- Whiteness as a foundation of mental health care
- Distrust of the medical industry
- Difficulty navigating the process
- Emotional hesitation
- Negative past experiences
LGBTQ+ people share similar barriers, which may also include:
- Coming out
- Rejection
- Trauma
- Substance use disorder
- Suicide
- Inadequate health care
In sum, experiences of anti-Blackness, homophobia and transphobia, undocumented immigration status, history of incarceration or substance use disorder, and other factors can create barriers to accessing mental health support for survivors from marginalized communities.
Ways to promote mental health and/or support those with mental illness:
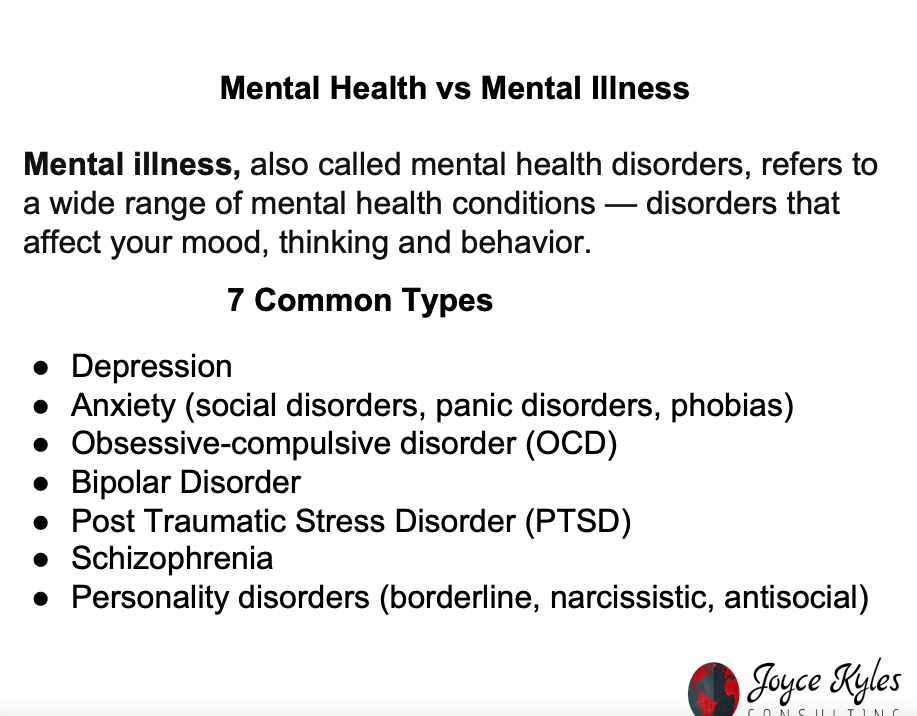 1) Understanding mental health vs mental illness.
1) Understanding mental health vs mental illness.
“Although the terms are often used interchangeably, poor mental health and mental illness are not the same. A person can experience poor mental health and not be diagnosed with a mental illness. Likewise, a person diagnosed with a mental illness can experience periods of physical, mental, and social well-being.”
Survivors may be experiencing one or both of these. It is important to understand the differences between the two. It equips advocates and providers with the proper knowledge and terminology. The video, Mental Health VS Mental Illness (What's The Difference?) further clarifies the distinctions.
2) Addressing the psychological effects of domestic and sexual violence.
Domestic violence and other lifetime trauma are associated with a wide range of health and mental health effects:
- There is a large and growing body of evidence documenting the associations between domestic violence and mental health conditions, including substance abuse (substance use disorders).
- On average, more than half of the women seen in mental health settings are or have been abused by an intimate partner.
- Common diagnoses among these women include post-traumatic stress disorder (PTSD), depression, and anxiety.
- PTSD among domestic violence survivors is between 31% and 84%, compared to about 3.5% of the general population.
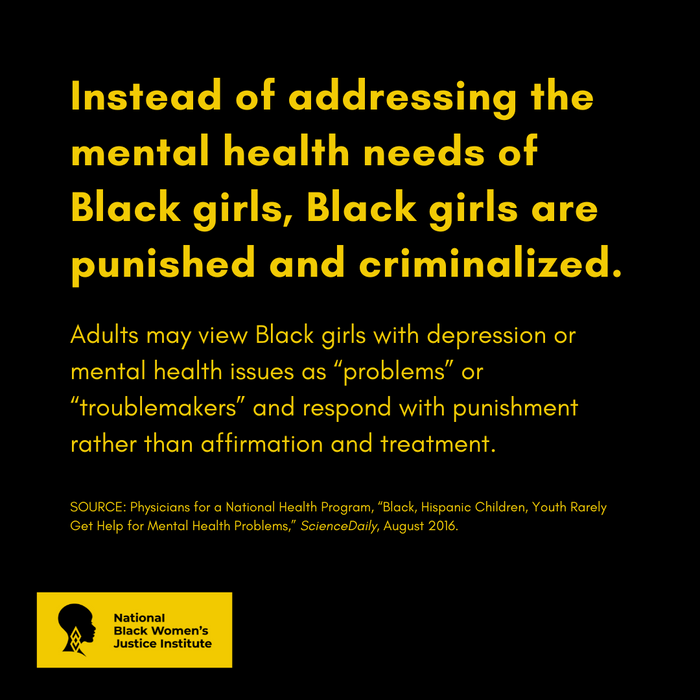
- Black girls experience discrimination related to both race and gender, which can impact mental health. Girls who experience gender-based violence such as sexual harassment tend to have an elevated risk of self-harm, suicidal thoughts, and feeling unsafe at school.
- Physicians working with Black patients were 33% less likely to engage in patient-centered communications than they were with white patients. Such discriminatory practices have been connected to patients’ increased psychological distress.
- Symptoms of depression can vary from one person to the next. New research shows that variation in depression symptoms could translate to underdiagnosis and missed care. For instance, health care providers may miss depression symptoms in Black women, resulting in underdiagnosis and undertreatment.
The National Center on Domestic Violence, Trauma & Mental Health provides a wealth of tools and resources to help advocates working with survivors who are experiencing trauma symptoms and/or mental health conditions.
3) Advocating for more funding.
“Sure, I have seen a lack of funding put into mental health for supporting survivors. This makes no sense. Studies have shown over decades the amount of damage that abuse does to an individual. Also, ACEs (Adverse Childhood Experiences) show how early intervention decreases an individual's risk level. But we still have little funding put into prevention. It's past time that we are reactive. We need to be proactive. Help is needed to provide the tools for individuals and families to establish, maintain, and cultivate healthy relationships for themselves and others.” – Phillis Lewis, CEO, of Love Doesn’t Hurt
According to the Domestic Violence Counts Survey conducted on September 7, 2022 by the National Network to End Domestic Violence (NNEDV):
- 85% of domestic violence programs across the country offered support/advocacy related to mental health in the 12 months prior to the survey.
- During that time period, therapy/counseling for adults were offered by 67% of programs, and 54% offered therapy/counseling for children or youth.
Sadly, the demand for help often exceeds the limited community resources available. Programs have reported drastic increases and new complexities in survivors’ mental health concerns since the COVID-19 pandemic. These concerns put additional strains on available services. And the healing process for survivors is delayed when programs do not have the resources to support them. With increased funding, programs can invest in specialized supports around mental health and substance abuse to help survivors in their healing path.
4) Providing survivors and advocates with safe spaces for mental health support.
A recent survey by the SOAR Collective found that 60% of advocates identify their survivorship as inspiration to work in the anti-violence movement. This means that anytime we support advocates, we are often also supporting survivors.
Advocates and providers give a lot of themselves. They maximize their level of service capacity. Survivors need to feel valued. They deserve exposure to support systems not always afforded to them due to the aforementioned barriers.
The 3-part webinar series, DVAM Webinar Series: #1Thing to #Care4Advocates Mind, Body, and Soul features tools and strategies for supporting advocates’ health and wellness, including ways to prioritize self-care and avoid burnout. Myself and other presenters explore how creating the conditions where advocates, especially those most marginalized, can thrive aligns with the commitment to No Survivor Justice Without Racial Justice.
5) Increasing the focus on awareness and treatment of marginalized survivors.
Because the majority of the domestic violence awareness movement has focused on heterosexual relationships, members of LGBTQ+ communities have been largely left out of the movement. But recent research shows that LGBTQ individuals fall victim to domestic violence at equal or even higher rates compared to their heterosexual counterparts.
 LGBTQ individuals who have experienced domestic violence may be at increased risk for mental health problems as well. As with the cisgender population, depression and anxiety are found to be significantly correlated with experiences of domestic violence among transgender and gender nonconforming individuals.
LGBTQ individuals who have experienced domestic violence may be at increased risk for mental health problems as well. As with the cisgender population, depression and anxiety are found to be significantly correlated with experiences of domestic violence among transgender and gender nonconforming individuals.
Also, studies confirm that the COVID-19 pandemic exacerbated risks and vulnerabilities faced by marginalized communities, including physical and mental health challenges. For example, a new study found that mental health and emotional wellness were among the greatest needs facing Black girls and gender-expansive youth in the foster care and juvenile legal system during the pandemic.
Increasing the focus on awareness and treatment of marginalized survivors is key. Survivors should not only have access to mental health care services, but access to quality and culturally competent mental health care. Survivors from marginalized groups may feel more comfortable speaking about their mental health needs with members of their own communities.
“We constantly hear from Black women and girls as a part of our programming and community that they are looking for culturally- and gender-responsive providers that understand and empathize with the unique risk factors and experiences that impact the mental health and wellbeing of Black women and girls. We also consistently hear requests to increase access to providers of color and additional ‘spaces’ and opportunities for healing and sisterhood as it pertains to mental healing and processing.” – Black Girls Smile, Inc.
Advocates at anti-violence organizations can be invaluable in connecting survivors with these relevant referrals. Resources such as BEAM, National Queer & Trans Therapists of Color Network, Therapy for Black Girls, The Loveland Foundation, and The Brown Therapist Network can aid advocates in making those connections.
Understanding the historic relationship between marginalized communities and mental health providers is also critical. Historically oppressed communities have been pathologized in psychology and medicine. Thus, survivors from marginalized groups may be more hesitant to seek help, given historical and current dehumanizing practices in mental health services.
For this reason, the National Center on Violence Against Women in the Black Community, also known as Ujima, emphasizes that to address the healing and wellbeing of Black women who are survivors of domestic violence, we must reconcile the factors that continue to have tangible and intangible effects on them. The Impact and Treatment of PTSD for Black Women Experiencing Intimate Partner Violence, a webinar hosted by Ujima, provides a deeper dive into the barriers, needs for support, and strategies that the gender-based violence movement should implement to support healing for Black survivors from historical induced trauma.
Conclusion
In conclusion, I would like to uplift two additional organizations:
- Love Doesn’t Hurt (LDH) provides services to victims of domestic and sexual violence in the lesbian, gay, bisexual, and transgender communities. Each month, they host a Love is Love Support Group. It provides a safe, affirming, and inclusive space for individuals who have experienced violence or trauma in the LGBTQ+ community. It is free of charge to attend.
- Crime Victims & Rape Crisis Center provides comprehensive services and resources to victims of crime; educates the community about victimization, trauma, and the incredible strength, resiliency, and hope of those impacted by crime; and equips and empowers the community with information and skills to live violence-free lives.
Both organizations recognize that advocates’ need for self-care and restoration is a must. Sandy Bromley, Deputy Director of Justice Programs for the Division of Community Services, and former Executive Director of the Crime Victims & Rape Crisis Center is adamant about the values of safety and well-being for herself and her staff.
“First, as one of our agency values – Safety & Well-being – we were purposeful about declaring that staff safety and well-being are as important as client safety and well-being so that our team members are able to be in a good place to provide good services. Second, to live out that value, we encourage staff to take 1 hour of intentional self-care each week. We are intentional about using the word intentional in this phrase. We want staff to plan out their self-care hour to pour back into themselves to sustain their work."
The intersecting traumas and “isms” faced by marginalized groups create barriers to healing and have a significant impact on mental health and overall wellness. In order to better support survivors within marginalized communities in addressing their mental health needs, advocates must understand that health equity is our work. Advocates must create the conditions that provide every survivor with the chance to enjoy good health and mental health. For that, we must center the needs and voices of those most marginalized. By adopting accessible, culturally sensitive, and trauma-informed approaches, we can be responsive to a wide range of people’s experiences, as well as more relevant to the people and communities that we serve.